Fighting resistant bacteria with viruses
Researchers at ETH Zurich modify enzymes from phages - natural enemies of bacteria - and send them specifically into infected tissue.
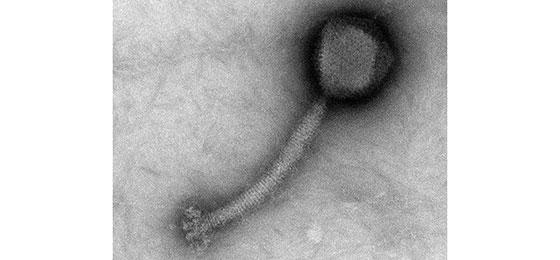
Staphylococcus aureus bacteriophage (photograph courtesy of J. Klumpp)
With the discovery of antibiotics in the mid-1900s, other approaches to treating infections – including phage therapy – were largely forgotten. But now that antibiotic-resistant bacteria are becoming an ever-greater problem, research has once again turned to phages. These viruses are natural – and deadly – enemies of bacteria.
Microbiologists Martin Loessner and Mathias Schmelcher of the Department of Public Health Sciences and Technology at ETH Zurich are exploiting this potential. “Today we have techniques for manipulating phages and the means for conducting medical investigations under controlled conditions”, says Loessner.
Punching through cell walls
In contrast to classical phage therapy, the Zurich researchers don’t work with whole phages. Instead, they focus on an enyzmes produced by phages called endolysins. Phages use these enzymes to punch holes in the cell walls of bacteria. This allows them to leave the cells after using them as hosts for their own reproduction. And because bacteria with heavily perforated cell walls die off, endolysins have great potential for controlling bacterial infections.
Endolysins also have another key advantage: so far as we know, bacteria are unable to mount any resistance to them. This is because the structure of the bacterial cell wall targeted by endolysins is highly conserved and cannot be altered without impairing the viability of the bacteria. In addition, endolysins can also attach to the cell wall from without and, unlike most antibiotics, do not need to penetrate inside the bacteria. This allows them to bypass many common resistance mechanisms.
Maximum effect through intelligent design
In the last few years, Loessner and Schmelcher have developed a range of potential new agents based on endolysins. “We have altered the natural building blocks of endolysins and reconfigured them like Lego bricks in new ways to create completely new, optimised enzymes”, says Schmelcher. For example, the new enzymes contain a component that binds to the cell wall of bacteria as well as other components that punch holes in the cell wall at various points. Other modifications – some of which are already being tested – could, for example, prevent an overly strong immune response in the patient or may prolong the circulation time of the enzyme in the blood.
From a library of more than 400 tailor-made enzymes, the research team has now pinpointed several promising candidates that are particularly effective against the bacterium Staphylococcus aureus in blood serum. This pathogen is responsible for many acute and chronic infections in humans, especially in its multiresistant form (MRSA).
Biological postcodes mark the spot
For even greater effectiveness, Loessner and Schmelcher have added short protein sequences to their compounds, which are intended to direct the endolysins specifically to the source of infection. “In this way, we want to ensure that the active ingredient is not distributed throughout the entire body, but rather is concentrated in the tissues and organs where it is really needed”, says Schmelcher. These sequences are, so to speak, biological postcodes that bind specifically to a certain type of tissue and introduce the agent inside the body’s cells – i.e. precisely where the bacteria are located.
In the meanwhile, the two researchers have already identified the appropriate postcodes for cells of the periosteum (bone membrane) and cardiac epithelium, both of which are tissue types in which staphylococci cause dangerous infections. Following installation of a hip implant, for example, the bacteria often form a biofilm on the bones that is particularly resistant to treatment with antibiotics. And in the heart, staphylococci attach themselves to the heart valves, where they then spread through the bloodstream and lead to life-threatening blood poisoning.
From basic research to treatment
Now that the researchers have successfully demonstrated the efficacy of their agents in Petri dishes, the next step is tests in living organisms. This will show whether the biological postcodes actually do deliver the agents to the correct address. To this end the microbiologists are working closely together with physician Annelies Zinkernagel of the Department of Infectious Diseases and Hospital Epidemiology at University Hospital Zurich.
“We have developed the basic principles, but we cannot carry out tests in mouse models without clinical practitioners”, says Loessner. “It’s a big advantage that the National Research Programme on antimicrobial resistance promotes collaboration between different groups.” Not least, these collaborations also benefit patients who depend on new treatments against bacterial infections.
